CHRONIC KIDNEY DISEASE (CKD) &END STAGE KIDNEY DAMAGE(ESKD)
 |
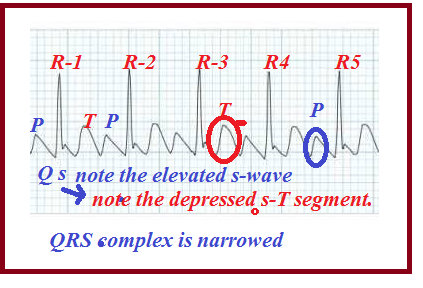
| Fig-1 |
Chronic Kidney Damage or CKD can be defined as the step by step or slow loss of kidney functions over a long time period of months or years.
The main culprits for this CKD are generally High Blood Pressure(HBP) and Diabetes Mellitus(DM)
.Both uncontrolled high B.P and high sugar can damage the kidneys as follows:-
High B.P. would reduce the amount of blood flow to the kidney and thereby the kidney becomes undernourished.
Similarly high blood sugar will damage the glomerular filter system by sugar deposits. Thus the nephron can gradually lose its filtering capacity.
All causes of acute kidney failure are also fit for chronic kidney damages.
High B.P. would reduce the amount of blood flow to the kidney and thereby the kidney becomes undernourished.
Similarly high blood sugar will damage the glomerular filter system by sugar deposits. Thus the nephron can gradually lose its filtering capacity.
All causes of acute kidney failure are also fit for chronic kidney damages.
STAGES:-
1. Normal or above the normal stage- GFR (Glomerular Filter Rate)-Above 100 ml/min)
2.Mild stage -(GFR-60 to 99 ml/min)
3A.Moderate- (GFR-49 to 59 ml/min)
3B.Moderate- (GFR-35 to 49 mi/min)
4. Severe stage- (GFR- 19 to 29 ml/min)
5.End-stage - (GFR-<19 ml/min)
The first two stages can be reversed if attended in time with proper treatments. But they are asymptomatic and escape silently like thieves from our attention. Once the stage entered the third to fourth level the disease cannot be reversed as almost 50% of the kidney functions are destroyed.
The first two stages can be reversed if attended in time with proper treatments. But they are asymptomatic and escape silently like thieves from our attention. Once the stage entered the third to fourth level the disease cannot be reversed as almost 50% of the kidney functions are destroyed.
Signs and Symptoms of CKD:-
1.Nausea and vomiting
2.Loss of hungry
3.Weakness and mental swings
4.Fatigue and tiredness
5. Frequent urination followed by reduced urination.
6.Foamy and bloody urine
7.Shortness of breath due to fluid collection in the lungs
8.Chest tightness and pain due to fluid collection in the heart.
9.High and uncontrolled B.P due to fluid retention.
10.Insomnia
11.Skin itching due to elevated wastes such as uric acid, urea, and phosphorus levels in the blood.
12.Muscle cramps.
Many of the above symptoms are not specifically due to CKD and a proper diagnosis should be done to confirm it.
Causes:-
1.Diabetes mellitus
2.Chronic High B.P.
3.Tubule Infections
4.Glomerular infections (Glomerulonephritis)
5.Vesicoureteral Reflux, a condition in which there is a reverse flow of urine back to the kidney.
6.Renal cysts
7.Prolonged urinary obstruction due to urethral pressure, and enlarged prostate.
8.Recurrent kidney infections.
Risk Factors:-
1.Old age
2.Smoking
3.Alcohol
4.Obesity
5.Uncontrolled cardiovascular diseases
6.Uncontrolled diabetes M
7.Hereditary Kidney disease
Complications:-
 |
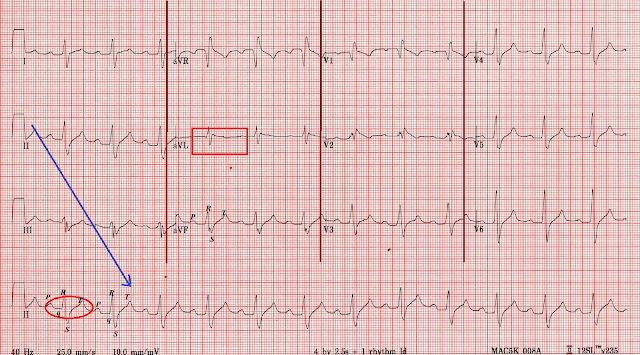
| Fig-2 |
Chronic kidney disease can affect almost all parts of the body due to the following complications.
1. Elevation of potassium levels can affect heart functions.
2. Elevation of phosphorus level can produce skin rashes.
3. Elevation of calcium level can produce kidney stones, and bone weakness and heart problems
4. Fluid retention can cause pulmonary and heart edema, ankles, and leg swellings, and high pressure.
5. Anemia prevails due to lack of erythropoietin production by the kidneys and thereby the production of RBC is reduced.
6.Reduced sexual drive, reduced fertility, and erectile dysfunctions.
7.CNS damages lead to mental health and other complications.
8. Damage to the immune system causes increased vulnerability of the body to infections.
9.Pericarditis-A condition in which more fluid collection in the pericardium, the upper covering of the heart. (See Fig-2) above.
The Concept of Anemia-Erythropoietin:-
Apart from functioning as an excretory organ kidney plays other important roles to maintain our body's health.
Blood needs regular synthesis of Red Blood Cells (RBC) every day to compensate for its loss on aging. Erythropoietin is an important catalyst to synthesize new RBCs by the bone marrow. Erythropoietin is secreted by the kidneys and liver. Liver secretion is predominant in childhood. Afterward kidney secretion of erythropoietin is predominant in adulthood. At ESKD kidneys lose almost 90% of the ability to produce erythropoietin and hence anemia develops rapidly.
Erythropoietin is produced by the interstitial fibroblasts in close association with the peritubular capillaries and the proximal convoluted tubule See Fig-3 above)
1.EPO is released into the blood circulation from the kidneys.
2.EPO tells the bone marrow to synthesize and release RBC.
3.RBC is released into the circulation. (Fig-3)
The erythropoietin (EPO) production is increased in a low oxygen atmosphere to produce more RBC. People living in high altitudes are subjected to produce high EPO production by the kidney as the availability of oxygen is low there.
1.EPO is released into the blood circulation from the kidneys.
2.EPO tells the bone marrow to synthesize and release RBC.
3.RBC is released into the circulation. (Fig-3)
The erythropoietin (EPO) production is increased in a low oxygen atmosphere to produce more RBC. People living in high altitudes are subjected to produce high EPO production by the kidney as the availability of oxygen is low there.
TESTS AND DIAGNOSES:-
1.EPO TEST;-
EPO test is not so important to confirm CKD since there are many other factors that cause the irregularities of the EPO level in the blood.
The high altitude where there is low oxygen density would increase the erythropoietin level in the blood.
Polycythemia (abnormal elevation of RBC in the blood due to bone marrow defects would lower the release of erythropoietin by the kidneys.
In the case of end-stage kidney damage (ESKD) the kidneys are fully disabled to produce EPO. Hence the EPO test may be a marker of the presence of ESKD.
The normal EPO level in the blood is 4 to 40 international units per liter (IU/L) of the blood.
Usually in kidneys the proximal convoluted tubule, the peritubular capillaries in the cortex are the areas where the interstitium produces EPO.
For an elaborate study click here
2. Diagnosis for ESKD involves a 24 hours urine test
3.Blood creatinine analysis:-Normal creatinine level is 0.7 to 1.2 mg/dl
4.Blood Urea Nitrogen tests:- Normal urea level is 14 to 25 mg/dl
The best marker to predict any type of kidney damage is the micro protein urea tests which we already described in previous chapters. To see that click here
KIDNEY INJURY MOLECULE (KIM)TEST:-
The most reliable and accurate diagnostic test to predict AKD and CKD is the KIM-1 test.
KIM is a transmembrane glycoprotein present in the epithelial layer of the proximal tubule.Normal urine contains 0 to 0.7ng/ml.But in the injured kidney the level raises above 3.7 ng/ml which predicts kidney damage.
The test is more accurate to indicate the presence of AKD but can also be used as a reliable marker test to predict CKD.
Diet control, dialysis followed by EPO injections, or kidney transplants are life-saving formulas for those who reached end-stage kidney disease(ESKD).
ERYTHROPOIETIN INJECTIONS:-
These are human recombinant erythropoiesis-stimulating injections that must be given to the kidney patients either in dialysis or not.
The injections should be given at least three times per week and the dosage should be determined by the doctor.
Availability:-1) 2000 units/ml
2) 3000 units/ml
3) 4000 units/ml
4) 10000 units/ml
The initial treatment should be started when the hemoglobin count falls below 10 gram per deciliter of the blood.
As the count raises reduce the dosage accordingly.
Usual Dosage:-50 to 100 units per kg via IV or SC route.
Hemodialysis & Peritoneal dialysis will be presented as separate posts in the future.
National Park Tweets - Curated tweets by TwitterDev
EPO test is not so important to confirm CKD since there are many other factors that cause the irregularities of the EPO level in the blood.
The high altitude where there is low oxygen density would increase the erythropoietin level in the blood.
Polycythemia (abnormal elevation of RBC in the blood due to bone marrow defects would lower the release of erythropoietin by the kidneys.
In the case of end-stage kidney damage (ESKD) the kidneys are fully disabled to produce EPO. Hence the EPO test may be a marker of the presence of ESKD.
The normal EPO level in the blood is 4 to 40 international units per liter (IU/L) of the blood.
Usually in kidneys the proximal convoluted tubule, the peritubular capillaries in the cortex are the areas where the interstitium produces EPO.
For an elaborate study click here
2. Diagnosis for ESKD involves a 24 hours urine test
3.Blood creatinine analysis:-Normal creatinine level is 0.7 to 1.2 mg/dl
4.Blood Urea Nitrogen tests:- Normal urea level is 14 to 25 mg/dl
The best marker to predict any type of kidney damage is the micro protein urea tests which we already described in previous chapters. To see that click here
KIDNEY INJURY MOLECULE (KIM)TEST:-
The most reliable and accurate diagnostic test to predict AKD and CKD is the KIM-1 test.
KIM is a transmembrane glycoprotein present in the epithelial layer of the proximal tubule.Normal urine contains 0 to 0.7ng/ml.But in the injured kidney the level raises above 3.7 ng/ml which predicts kidney damage.
The test is more accurate to indicate the presence of AKD but can also be used as a reliable marker test to predict CKD.
Diet control, dialysis followed by EPO injections, or kidney transplants are life-saving formulas for those who reached end-stage kidney disease(ESKD).
ERYTHROPOIETIN INJECTIONS:-
These are human recombinant erythropoiesis-stimulating injections that must be given to the kidney patients either in dialysis or not.
The injections should be given at least three times per week and the dosage should be determined by the doctor.
Availability:-1) 2000 units/ml
2) 3000 units/ml
3) 4000 units/ml
4) 10000 units/ml
The initial treatment should be started when the hemoglobin count falls below 10 gram per deciliter of the blood.
As the count raises reduce the dosage accordingly.
Usual Dosage:-50 to 100 units per kg via IV or SC route.
Hemodialysis & Peritoneal dialysis will be presented as separate posts in the future.