ACUTE KIDNEY FAILURE(AKF or AKD)
Acute kidney damage is a condition in which the kidneys are suddenly unable to clean your blood from harmful wastes, dangerous metabolites, and thereby let them accumulate in your body to a dangerous life-threatening level.
The condition develops in a short period of time in a few days or even in a few hours and can be fatal and need intensive hospital care.
Acute kidney failure or damage may sometimes be reversed to a normal condition if there are no other problems.
AKD may be confirmed when there is a 50 to >50% increase in serum creatinine levels.
AKD may be confirmed when there is a 50 to >50% increase in serum creatinine levels.
 |
| Fig 1 |
A sudden episode of kidney failure occurs for the following reasons.
1.Drugs of abuses like alcohol, narcotics, pain killers, antibiotics, and any poisonous drug whose metabolite can harm kidneys.
Alcohol over usage can cause kidney muscular necrosis as its metabolites such as acetaldehyde without further dehydration to acetic acid may leak from the liver and cause necrosis to the kidney tubular cells.
Over drink of alcohol may cause high B.P which is harmful to the kidney.
2.Pain Killer abuse. Non-Steroidal Anti Inflammatory Drugs can cause kidney damages if overdosed. They inhibit the production of important biological mediators such as prostaglandins. Prostaglandin PgE2 and Prostacyclin PgL2 are the important biological mediators that cause free renal blood flow by dilating the blood vessels and thereby facilitate and increase glomerular filtration.NSAIDs such as ibuprofen, naproxen, phenoxybenzamine, indomethacin, and aspirin are all inhibiting cyclooxygenase (COX-1 &2)and thereby inhibiting the prostaglandin synthesis.
3.Acute tubular necrosis. This condition can happen due to the consumption of foods, drinks, and drugs which can be converted into harmful excretory products or metabolites.
(e.g)Iodine contaminated contrast media for radio analysis.
After an intramuscular administration of iodinated contrast media, some patients reported within a few days of acute kidney injury developed which is
notified by an increase in creatinine and blood urea level above the normal.
In the above Table, a few examples have been described for your reference.
1. Heavy consumption of ethanol can result in sudden acute renal injury in many ways.
The liver metabolizes ethanol into acetaldehyde by the enzyme alcohol dehydrogenase. Acetaldehyde is further metabolized by aldehyde dehydrogenase to harmless acetic acid which is decomposed to water and carbon dioxide.
But in some unhealthy situations of liver damage for example during hypothyroidism the liver may not properly metabolize acetaldehyde due to lack of aldehyde dehydrate. In this case the unmetabolized acetaldehyde can reach the kidneys and harm both kidneys as well as the liver. Remember acetaldehyde is highly carcinogenic.
Heavy consumption of alcohol can raise your B.P.and sugar in the blood and thereby reducing the blood supply to the kidneys and thereby injure them.
2. Methanol also produces dangerous metabolites like formaldehyde and formic acid both are harmful to the liver as well as to kidneys.
3. All opioids used as pain killers, diarrhea, and cough suppressants are all harmful to the kidneys.
Codeine phosphate, an opioid that is used in cough syrups as an antitussive (cough suppressant) agent can harm your kidney by its metabolites morphine, norcodeine, and codeine-6-phosphate.
4. Aminoglycosides such as neomycin, tobramycin, gentamicin, and streptomycin are all excreted by the kidney unchanged. The damage is mainly at the proximal tubule cells after passing through the glomerular filtration.
5. Heavy metals such as cadmium, chromium, and mercury are all excreted through the kidneys unchanged. Cadmium poisoning is very common in our life. Rice produced by using phosphate fertilizers, usage of plastics, pigments, and platings,
batteries, exposing to sewage sludge are all the possible man-made sources of cadmium poisoning. Cigarette smoking is one of the sources to get cadmium exposure to heavy smokers. Chronic exposure to cadmium may damage your kidney.
5. Pain killers such as ibuprofen(brufen), naproxen(Proxen), aspirin are harming the kidneys by inhibiting the synthesis of biological mediators prostaglandin, and prostacyclin.
1.Drugs of abuses like alcohol, narcotics, pain killers, antibiotics, and any poisonous drug whose metabolite can harm kidneys.
Alcohol over usage can cause kidney muscular necrosis as its metabolites such as acetaldehyde without further dehydration to acetic acid may leak from the liver and cause necrosis to the kidney tubular cells.
Over drink of alcohol may cause high B.P which is harmful to the kidney.
2.Pain Killer abuse. Non-Steroidal Anti Inflammatory Drugs can cause kidney damages if overdosed. They inhibit the production of important biological mediators such as prostaglandins. Prostaglandin PgE2 and Prostacyclin PgL2 are the important biological mediators that cause free renal blood flow by dilating the blood vessels and thereby facilitate and increase glomerular filtration.NSAIDs such as ibuprofen, naproxen, phenoxybenzamine, indomethacin, and aspirin are all inhibiting cyclooxygenase (COX-1 &2)and thereby inhibiting the prostaglandin synthesis.
3.Acute tubular necrosis. This condition can happen due to the consumption of foods, drinks, and drugs which can be converted into harmful excretory products or metabolites.
(e.g)Iodine contaminated contrast media for radio analysis.
After an intramuscular administration of iodinated contrast media, some patients reported within a few days of acute kidney injury developed which is
notified by an increase in creatinine and blood urea level above the normal.
ETIOLOGY
 |
| Fig 1(Table) |
1. Heavy consumption of ethanol can result in sudden acute renal injury in many ways.
The liver metabolizes ethanol into acetaldehyde by the enzyme alcohol dehydrogenase. Acetaldehyde is further metabolized by aldehyde dehydrogenase to harmless acetic acid which is decomposed to water and carbon dioxide.
But in some unhealthy situations of liver damage for example during hypothyroidism the liver may not properly metabolize acetaldehyde due to lack of aldehyde dehydrate. In this case the unmetabolized acetaldehyde can reach the kidneys and harm both kidneys as well as the liver. Remember acetaldehyde is highly carcinogenic.
Heavy consumption of alcohol can raise your B.P.and sugar in the blood and thereby reducing the blood supply to the kidneys and thereby injure them.
2. Methanol also produces dangerous metabolites like formaldehyde and formic acid both are harmful to the liver as well as to kidneys.
3. All opioids used as pain killers, diarrhea, and cough suppressants are all harmful to the kidneys.
Codeine phosphate, an opioid that is used in cough syrups as an antitussive (cough suppressant) agent can harm your kidney by its metabolites morphine, norcodeine, and codeine-6-phosphate.
4. Aminoglycosides such as neomycin, tobramycin, gentamicin, and streptomycin are all excreted by the kidney unchanged. The damage is mainly at the proximal tubule cells after passing through the glomerular filtration.
5. Heavy metals such as cadmium, chromium, and mercury are all excreted through the kidneys unchanged. Cadmium poisoning is very common in our life. Rice produced by using phosphate fertilizers, usage of plastics, pigments, and platings,
batteries, exposing to sewage sludge are all the possible man-made sources of cadmium poisoning. Cigarette smoking is one of the sources to get cadmium exposure to heavy smokers. Chronic exposure to cadmium may damage your kidney.
5. Pain killers such as ibuprofen(brufen), naproxen(Proxen), aspirin are harming the kidneys by inhibiting the synthesis of biological mediators prostaglandin, and prostacyclin.
Symptoms:-
The following are the symptoms of acute kidney failure.
1.Reduced urine output.Water retention and accumulation in the body.Swelling of the ankles, legs foot, and fingers.
2.Blood in the urine.
3.Tiredness and fatigue
4.Skin itching and necrosis
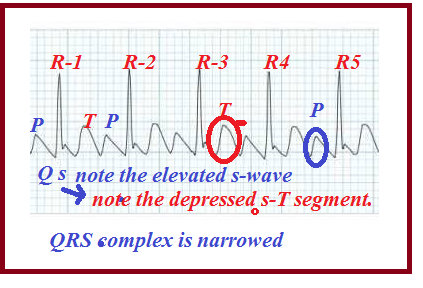
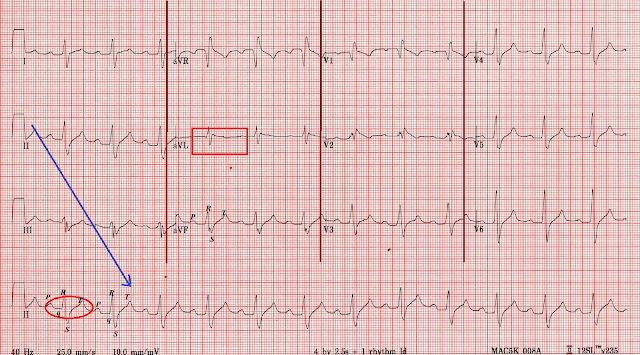
5.Cardiovascular diseases due to water accumulation inside the pericardial space.Arrhythmias.
6.Shortness of breath due to fluid accumulation in the lungs.
7.Nausea
8.Mood disturbances
9.Weakness.
10.Seizures and coma.
1.If the condition which slows the blood flow to the kidneys is solved. For example, blood and fluid loss. This can be corrected by proper blood transfusion and fluid infusion.
2.Discontinuation of the usage of painkillers
3.Immediate care of heart and liver diseases
4. Change B.P medication from ARB inhibitors (Losartan) or ACE inhibitors (Enalapril)to any other alternative medicine as ARB, and ACEI disturbs the aldosterone, vasopressin and adrenergic pathways and thereby harm kidney functions.
5.Urinary infection if any should be treated in time.
6. Severe dehydration due to diarrhea or vomiting, loss of fluid should be corrected immediately by drinks of infusion. The loss of electrolytes should be compensated.
7. Anaphylaxis and other allergic conditions should be cared for in time.
8. Avoid alcohol, tobacco, opioids, cocaine, like drugs of abuse.
9. Avoid amphetamines.
10. Take care of your prostate.
11. In sudden hemorrhages or blood loss due to accidents blood should be immediately compensated by infusion.
Continued...
6.Shortness of breath due to fluid accumulation in the lungs.
7.Nausea
8.Mood disturbances
9.Weakness.
10.Seizures and coma.
DIAGNOSIS:-
1.A.URINARY EVALUATION:-In AKD changes the blood creatinine level is not sensitive for early diagnosis.
Urinary levels of
a)Kidney Injury Molecule-1(KIM-1)
b)N-acetyl-β-D-glucosaminidase(NAG)
c)matrix metalloproteinase-9(MMP-9)
are evaluated as biomarkers for the detection of AKD.
AKD is often seen in the setting of multiple organs failure and sepsis.
The top and noninvasive biomarker is the KIM-1 biomarker. This is the more common biomarker for the early detection of AKD. This is a transmembrane protein. This is not detectable in normal kidney tissue or urine. But in dedifferentiated (PCT)epithelial cells and urine after an ischemic or toxic injury and in renal cancer this biomarker is expressed at a high level.
The NAG biomarker takes the next important biomarker place.
The least sensitive is the result of the MMP-9 biomarker.
The absence of sensitive biomarkers the diagnosis for early detection of AKD has had impaired and detrimental results. These biomarkers are micro molecules should be absent in the urine in normal persons
Urine tests to assess kidney diseases are usually performed with 24 hours of urine collection. To collect the sample the first urine which empties the bladder should be discarded and the next 24-hour urine should be collected for the tests.
1.B.Urinary Minerals Level.:-
The normal urine potassium level is 25 to 125 milliequivalent per liter. (mEq/L). But in case of AKD, this level goes down to below 25 mEq/L.A. Serum potassium test should be done to confirm the rise in potassium level above the normal limit(3.6 to 5.2 mmol/L)
(1mEq of potassium=39mg)
(To convert mmol/L to mg/dL multiply the figure by 18
To convert mg/dL to mmol/L, divide the figure by 18)
Similarly calcium in the urine (100 to 300 mg/day)should be done.
Urine magnesium should be less than 24 mg in a 24-hour urine collection.
Similarly, phosphorus should be measured in a 24 urine collection
2.Serum Creatinine Tests:
If the serum creatinine levels are above 3mg per deciliter then it could be assessed as there are epithelial damages and dedifferentiation in tubular tissues through which the filtered creatinine is leaked passively back into the blood. Another reason is if there are inflammations in the Bowman's capsules as in the case of glomerulonephritis which results in improper creatinine and urea filtration.
3.Blood Urea Nitrogen (BUN):-
The normal serum BUN level is between 7 to 25 mg per deciliter of the blood. In the case of AKD and CKD this may elevate beyond 30 mg/dL.
The NAG biomarker takes the next important biomarker place.
The least sensitive is the result of the MMP-9 biomarker.
The absence of sensitive biomarkers the diagnosis for early detection of AKD has had impaired and detrimental results. These biomarkers are micro molecules should be absent in the urine in normal persons
Urine tests to assess kidney diseases are usually performed with 24 hours of urine collection. To collect the sample the first urine which empties the bladder should be discarded and the next 24-hour urine should be collected for the tests.
1.B.Urinary Minerals Level.:-
The normal urine potassium level is 25 to 125 milliequivalent per liter. (mEq/L). But in case of AKD, this level goes down to below 25 mEq/L.A. Serum potassium test should be done to confirm the rise in potassium level above the normal limit(3.6 to 5.2 mmol/L)
(1mEq of potassium=39mg)
(To convert mmol/L to mg/dL multiply the figure by 18
To convert mg/dL to mmol/L, divide the figure by 18)
Similarly calcium in the urine (100 to 300 mg/day)should be done.
Urine magnesium should be less than 24 mg in a 24-hour urine collection.
Similarly, phosphorus should be measured in a 24 urine collection
2.Serum Creatinine Tests:
If the serum creatinine levels are above 3mg per deciliter then it could be assessed as there are epithelial damages and dedifferentiation in tubular tissues through which the filtered creatinine is leaked passively back into the blood. Another reason is if there are inflammations in the Bowman's capsules as in the case of glomerulonephritis which results in improper creatinine and urea filtration.
3.Blood Urea Nitrogen (BUN):-
The normal serum BUN level is between 7 to 25 mg per deciliter of the blood. In the case of AKD and CKD this may elevate beyond 30 mg/dL.
CORRECTIONS
Kidney damage in a short period can some times be reverted to normal if it is due to the following causes.1.If the condition which slows the blood flow to the kidneys is solved. For example, blood and fluid loss. This can be corrected by proper blood transfusion and fluid infusion.
2.Discontinuation of the usage of painkillers
3.Immediate care of heart and liver diseases
4. Change B.P medication from ARB inhibitors (Losartan) or ACE inhibitors (Enalapril)to any other alternative medicine as ARB, and ACEI disturbs the aldosterone, vasopressin and adrenergic pathways and thereby harm kidney functions.
5.Urinary infection if any should be treated in time.
6. Severe dehydration due to diarrhea or vomiting, loss of fluid should be corrected immediately by drinks of infusion. The loss of electrolytes should be compensated.
7. Anaphylaxis and other allergic conditions should be cared for in time.
8. Avoid alcohol, tobacco, opioids, cocaine, like drugs of abuse.
9. Avoid amphetamines.
10. Take care of your prostate.
11. In sudden hemorrhages or blood loss due to accidents blood should be immediately compensated by infusion.
Continued...